Tsinghua researchers recently reported on an unfavorable feedback loop by which a tumor can evade the immune system, and how immunotherapy works in some cancer patients.
Tumor cells can produce immune checkpoint molecules to mask themselves from the immune system. Immunotherapy targeting these molecules, which is named immune checkpoint blockade therapy, has shown great promise in the fight against cancer – some patients have even been cured. Unfortunately, immunotherapy has worked only in a small fraction of patients. Further mechanistic studies are urgently required to understand which kind of patients are being benefited, and more importantly, to explore how more patients can benefit from the therapy.
PD-L1 is one of the most important immune checkpoint molecules. It is commonly believed that tumor cells produce PD-L1 to interact with killer T cells, thus preventing T cells from damaging the tumor. In fact, assays determining the level of PD-L1 on tumor cells have been approved by the U.S. Food and Drug Administration (FDA) as a companion diagnostic assay to determine whether a patient can benefit from the therapy or not. However, only less than half of the PD-L1 positive patients respond to the therapy. On the other hand, some PD-L1 negative patients still respond well. And it remains unclear why.
In the current study, the researchers first measured PD-L1 levels in the tumors. They found that, compared to tumor cells, PD-L1 level is much higher in immune cells, especially in dendritic cells. The dendritic cell is an immune cell that plays an important role in antitumor immunity by taking up tumor debris, presenting it to the killer T cells and telling them how to separate tumor cells from normal healthy cells. By utilizing novel genetic modified-mouse models, the researchers showed that PD-L1 on dendritic cells dramatically dampens the antitumor immune response.
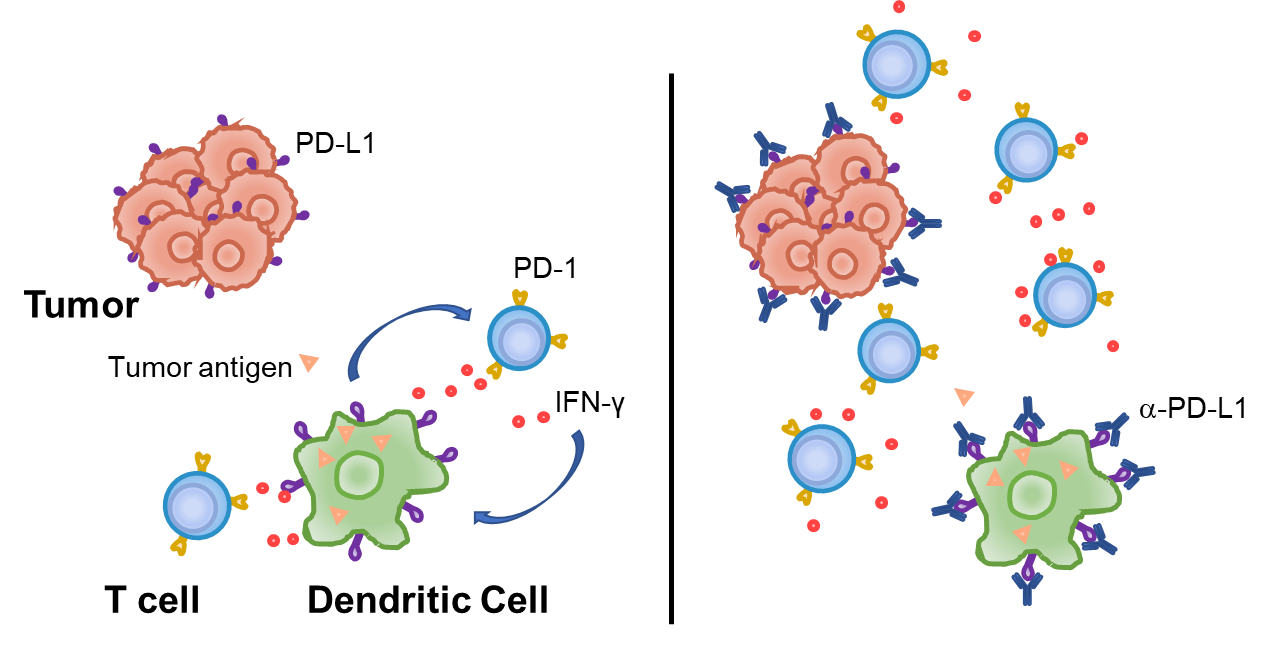
Furthermore, the study found that dendritic cells do not produce high levels of PD-L1 in healthy mice. When they contact with T cells, T cells will become activated and begin to produce interferon-gamma, a signaling cytokine that can both kill tumor cells and activate other components of the immune system. Meanwhile, interferon-gamma drives dendritic cells to produce PD-L1, and the latter dampens further activation of T cells. Under normal conditions, such processes serve as a feedback loop to prevent over-activation of the immune system, which might lead to auto-immune diseases. In the case of a tumor, however, it greatly suppresses the anti-tumor immunity and prevents the clearance of the tumor. This might be the reason why clinical responses of immune checkpoint blockade therapy are observed in patients where tumor cells do not produce PD-L1 – if their dendritic cells produce PD-L1, they might benefit from immunotherapy as well.
The study, led by Tang Haidong, a principal investigator in the School of Pharmaceutical Sciences, was published in Nature Communications entitled “PD-L1 on dendritic cells attenuates T cell activation and regulates response to immune checkpoint blockade.” The study can be accessed via the following link: https://www.nature.com/articles/s41467-020-18570-x.
Source: School of Pharmaceutical Sciences
Editors: John Obrich, Sangeet Sangroula, Lin Yuan
Cover Photo: Cang Linan



